Zika Seroprevalence of 2.4% in Postpartum Women

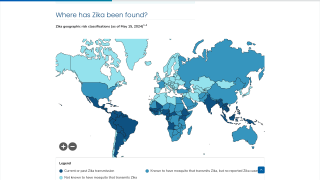
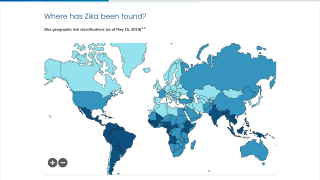
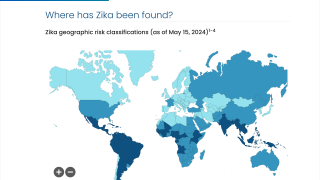
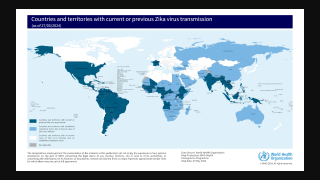
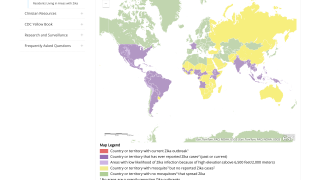
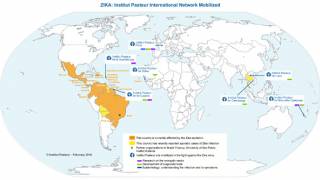
Over the past decade, the Zika virus has been found in over 50 countries and territories in the Region of the Americas.
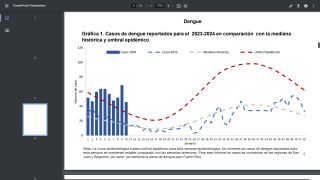
As of May 24, 2025, Zika virus (ZIKV) remains a significant public health concern in Brazil, with over 11,500 cases reported this year.
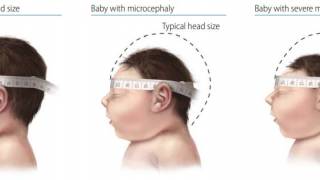
While most people recover from this mosquito-transmitted disease, pregnant women and their unborn children may become infected, leading to serious health issues.
Researchers have stated that understanding population serological status, particularly in pregnant women, is vital for estimating the spread of this virus.
A research article published by the Journal of Medical Virology on May 21, 2025, assessed ZIKV seroprevalence in pregnant women and the transplacental transfer of antibodies to their newborns, crucial for early-life protection.
Effective transplacental transfer of specific ZIKV antibodies from mothers to newborns was observed.
A cross-sectional seroprevalence study was conducted with 601 postpartum women and their newborns in São Paulo city, Brazil, post-ZIKV fever outbreak.
Paired maternal and umbilical blood samples were collected for ZIKV antibody testing. ZIKV neutralizing antibodies (nAbs) were detected in 2.4% of these women.
Maternal and neonatal characteristics were associated with seropositivity for ZIKV and the antibody transfer to neonates. Maternal place of birth, parity, education level, and prenatal Toxoplasmosis serology were identified as risk factors associated with ZIKV infection.
Low seroprevalence of ZIKV antibodies in the study population indicates a high vulnerability to infection by these viruses.
The low ZIKV seroprevalence observed in this study contrasts sharply with higher rates reported in the Northeast of Brazil, with 63% in pregnant women in Salvador (2015–2016) and 30% among Bolivian blood donors (2016–2017).
This study's findings offer a comprehensive understanding of the antibody transfer dynamics in the context of ZIKV infection. This understanding is paramount, as it can potentially inform vaccine development strategies in endemic regions and guide the development of more effective neonatal infection prevention measures.
Published in JAMA Network Open in January 2025, a population-based study of mortality rates among 11.4 million children born with a severe Zika virus infection had a strikingly higher risk of overall and cause-specific mortality.
Young children with congenital Zika syndrome (CZS) had a 13-fold higher risk of death compared with those without CZS. This study found that the cause-specific mortality hazard ratio was 30.28.
The U.S. CDC's updated Yellow Book says healthcare professionals should know how to diagnose, treat, and prevent Zika in international travelers, especially pregnant women.
The CDC writes providers should 'carefully evaluate pregnant women with laboratory evidence of Zika virus infection; closely manage these patients during pregnancy and carefully evaluate live-born infants for clinical features associated with intrauterine infection.'
While an innovative Zika vaccine candidate is conducting clinical trials in 2025, no vaccine has been approved.
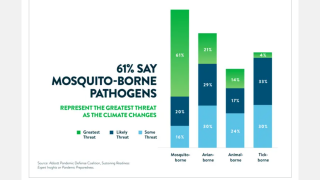
Researchers recently estimated that mosquitoes are carrying the Zika virus into new regions, and approximately 1.3 billion people could be affected by Zika by the year 2050.
The Pan American Health Organization writes, 'The decision to travel to a country with a history of Zika circulation should be based on a personal risk assessment, done in conjunction with the traveler's healthcare provider, that accounts for individual risk factors for severe outcomes from the possibility of a Zika infection.'
Our Trust Standards: Medical Advisory Committee






.jpg)








.jpg)